Hmm … it looks like your browser is out of date.
Let’s update your browser so you can enjoy a faster, more secure site experience.
2026 UHC Dual Complete PA-S3 (HMO-POS D-SNP)
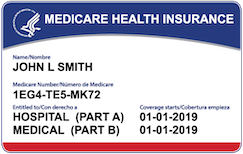
Medicare
What is a dual special needs plan?
H3113-016 -000
Monthly premium: $0.00 *
*Your costs may be as low as $0, depending on your level of Extra Help.
Our plan is a Medicare Advantage HMO Plan (HMO stands for Health Maintenance Organization) with a Point-of-Service (POS) option approved by Medicare and run by a private company. "Point-of-Service" means you can use providers outside the plan's network for an additional cost. If you have full Medicaid benefits or are a Qualified Medicare Beneficiary, this plan includes a $328 monthly credit for OTC, healthy food, and utilities, $0 prescription drugs, and other valued extras.
This plan is available in the following counties:
Allegheny, Armstrong, Beaver, Bedford, Berks, Blair, Bucks, Butler, Cambria, Chester, Clarion, Crawford, Cumberland, Dauphin, Elk, Erie, Fayette, Forest, Greene, Indiana, Jefferson, Lackawanna, Lancaster, Lawrence, Lebanon, Lehigh, Luzerne, Mercer, Monroe, Montgomery, Somerset, Venango, Warren, Washington, Westmoreland, and York.
- 2026 UHC Dual Complete PA-S3 (HMO-POS D-SNP)
1-844-812-5967 TTY: 711 8 a.m.-8 p.m. local time, 7 days a week
Find providers and coverage for this plan.
Search for doctors, hospitals, and specialists.
Search for providers, clinics and treatment centers.
Find a dentist near you.
Find a pharmacy near you.
Find medications covered by this plan.
Benefits & features
$2,500 dental allowance for covered services like cleanings, fillings, x-rays and crowns
$300 credit every month for OTC, plus healthy food and utilities for qualifying members
$200 allowance for one pair of glasses or contacts, plus $0 copay for a routine eye exam
$2,200 allowance for a broad selection of OTC and brand-name hearing aids
$0 copay for 36 one-way trips to or from doctor visits and the pharmacy
Fitness benefit
Free gym membership at core and premium locations
Routine foot care
4 foot care visits for nail trims and other covered preventive care
No cost medical services
$0 copay for primary care, hospital stays and specialist visits
Prescription drug coverage
$0 copay for Tier 1 prescriptions
Provider network
PCP-guided care plus access to our large provider network
Benefits, features and/or devices may vary by plan/area.
Limitations, exclusions and/or network restrictions may apply.
OTC, food and utility benefits have expiration timeframes.
Review your Evidence of Coverage (EOC) for more information.
The healthy food and utilities benefit is a special supplemental benefit only available to chronically ill enrollees with a qualifying condition, such as diabetes, cardiovascular disorders, chronic heart failure, chronic high blood pressure and/or chronic high cholesterol, and who also meet all applicable plan coverage criteria. There may be other qualified chronic conditions not listed.
If your plan offers out-of-network dental coverage and you see an out-of-network dentist, you might be billed more. Network size varies by local market.
Review your plan Drug List (Formulary) on UHC.com/Medicare for a list of covered prescription drugs, including those on Tier 1.
Annual routine eye exam and an allowance for contacts or one pair of frames, with standard (single, bi-focal, tri-focal or standard progressive) lenses covered in full every year. Review your Evidence of Coverage (EOC) for more information.
The plan only covers hearing aids from a UnitedHealthcare Hearing network provider. Other hearing exam providers are available in the UnitedHealthcare network.
The fitness benefit and gym network varies by plan/area and participating locations may change. The fitness benefit includes a standard fitness membership at participating locations. Not all plans offer access to premium locations. Consult your doctor prior to beginning an exercise program or making changes to your lifestyle or health care routine.
Network size varies by local market and exclusions may apply.
Referrals may be needed to see network specialists.
Routine transportation not for use in emergencies.
A trip is one-way and roundtrip is two trips.
UHC Dual Complete PA-S3 (HMO-POS D-SNP)
Monthly plan premium for people who get Extra Help from Medicare to help pay for their prescription drug costs
If you get Extra Help from Medicare to help pay for your Medicare prescription drug plan costs, your monthly plan premium will be lower than what it would be if you did not get Extra Help from Medicare. The amount of Extra Help you get will determine your total monthly plan premium as a member of our Plan.
This table shows you what your monthly plan premium will be if you get Extra Help.
| Your level of Extra Help | Monthly premium* |
|---|---|
| 100% | $0.00 |
*This does not include any Medicare Part B premium you may have to pay.
If you aren’t getting Extra Help, you can see if you qualify by calling:
- 1-800-Medicare or TTY users call 1-877-486-2048 (24 hours a day/7 days a week),
- Your State Medicaid Office, or
- The Social Security Administration at 1-800-772-1213. TTY users should call 1-800-325-0778 between 7 a.m. and 7 p.m., Monday through Friday.
Your health care needs are unique. These documents can help you make sure you get the right coverage.
Documents include Annual Notice of Changes, Evidence of Coverage, Formularies, Medicare Plan Star Ratings, Provider Directories, Summary of Benefits, Other downloadable resources.
Learn more about dual special needs plans
Learn more
UHC Dual Complete PA-S3 (HMO-POS D-SNP)